GLASGOW COLORECTAL CENTRE
Scotland’s Best Private Colorectal Surgery & Colonoscopy Clinic
info@colorectalcentre.co.uk
If you have any questions, call Catherine on 0735 506 6597

© Glasgow Colorectal Centre. All Rights Reserved

 Book an Appointment
Book an Appointment
Any questions? Call Catherine on 0735 506 6597
Info@colorectalcentre.co.uk

Anal abscess & anal fistula
Causes, symptoms and treatment

If you have any additional questions about anorectal abscesses and fistulas or other colorectal issues, your own GP is often the best first port of call.
If appropriate, they will be able to arrange a referral to a colorectal specialist centre such as the Glasgow Colorectal Centre.
What is an anal abscess or fistula?
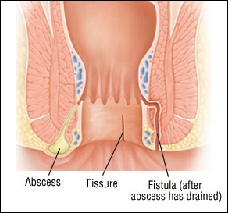
An anal abscess develops near the anus or back passage. Typically, it develops fairly quickly and gives rise to pain in the rectum or anus combined with fever, chills, and generally feeling unwell. There may be an obvious painful swelling alongside the anus or back passage.
An anal fistula is almost always the result of a previous abscess. A fistula connects a previously infected anal gland to the skin on the buttocks outside the anus. Symptoms include a persistent discharge from an opening or sinus near the anus. It may arise at the site of discharge of a perianal abscess.
What causes a perianal abscess abscess?
Just inside the anus are small glands. When these glands get clogged, they may become infected and an abscess can develop.
An abscess results from an acute infection in the anal glands, when bacteria or foreign matter enters the tissue through the gland. Certain conditions -
What causes a fistula in ano?
An anal fistula usually develops after an anal abscess (a collection of pus) bursts, or when an abscess has not been completely treated. After an abscess has been drained, a tunnel may persist connecting the anal gland from which the abscess arose to the skin. If this occurs, persistent drainage from the outside opening may indicate the persistence of this tunnel. If the outside opening of the tunnel heals, recurrent abscess may develop.
A fistula can also be caused by conditions that affect the intestines, such as Crohn's disease or ulcerative colitis. As many as 50% of people with Crohn’s disease get an anal fistula. Up to 30% of people with HIV (a virus that attacks the body's immune system) will also develop an anal fistula.
Anal fistulae are more common in men, mostly between the ages of 20 and 40. A study published in 2007 that looked at four different European countries, including England, found that there are between one and three cases of anal fistulae for every 10,000 people.
What are the symptoms of an abscess or fistula?
An abscess is usually associated with symptoms of pain and swelling around the anus. Individuals may also experience fatigue, fevers and chills. Symptoms related to the fistula include
- Discharge of pus for an opening near the anus (discharge may relieve the pain)
- Pain and discomfort in the anal region
- Irritation of skin around the anus
- Passing some blood with the discharge
- Fever
- Feeing poorly in general (malaise)
Does an abscess always become a fistula?
Around 1/3 of patients who get an abscess will never get another abscess after the initial treatment. One third will get further abscesses. Finally, around 1/3 to ½ will go on to develop a fistula. Unfortunately, there is really no way to predict if this will occur.
How is a perianal abscess and fistula in ano diagnosed?
Usually, either condition can be diagnosed with a careful clinical examination by a specialist. On occasion, it may be necessary to arrange specialist scans (e.g. MRI, CT or ultrasound scan) or alternatively, your specialist may need to bring you in for an examination under anaesthetic in order to get a complete assessment of the anal region.
How is a perianal abscess treated?
On occasion, an abscess may “burst” spontaneously onto the skin and start to drain pus. This is more likely if the abscess develops at the site of an old abscess or previous operation site to drain an old abscess.
New abscesses may require an operation to drain the pus. The abscess is treated by making an opening in the skin near the anus to drain the pus from the infected cavity and thereby relieve the pressure. Very superficial abscesses can sometimes be drained under local anaesthetic. However, many patients and surgeons prefer to perform drainage of such abscesses under general anaesthetic. Although this can often be performed as a day case or overnight stay, on occasion, very large abscesses in patients prone to more serious infections, such as diabetics or people with decreased immunity may require more a prolonged stay in hospital. Antibiotics are a poor alternative to draining the pus, because antibiotics do not penetrate the fluid within an abscess.
How can a fistula be treated?
Surgery is necessary to cure an anal fistula. Although fistula surgery is usually relatively straightforward, the potential for complication exists, and is preferably performed by a specialist in colon and rectal surgery. It may be performed at the same time as the abscess surgery, although fistulas often develop four to six weeks after an abscess is drained, sometimes even months or years later.
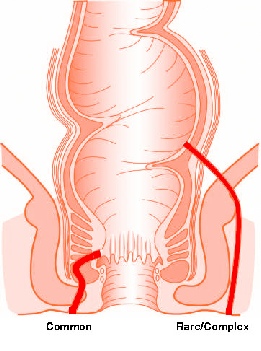
Your surgeon may decide to perform an initial assessment of the fistula to identify the openings and assess if the fistula is travelling deeply through the sphincter muscle. Not infrequently, surgery is performed as a staged series of operations. The first step may be passing a stitch (called a Seton suture) along the fistula in order to allow any residual abscess to drain. Definitive surgery is often performed 6-
Many different operations have been described to treat anal fistulas. You surgeon will discuss with you which operation they feel is best for your fistula. When deciding, your surgeon will take into account a number of factors including the depth of the fistula through the sphincter muscle, whether you suffer from other bowel conditions such as Crohn’s disease, your sex (the sphincter muscle in female patients is not as bulky as in men) and for female patients, whether they have had or intend to have children. Division of too much muscle might lead to impaired sphincter control and faecal incontinence.
Other methods or treating the fistula may be recommended by your surgeon. The most common operation that are performed are outline below
- Fistulotomy. This is frequently used and involves cutting open the whole length of the fistula in order for the surgeon to flush out the contents. This heals after one to two months into a flattened scar.
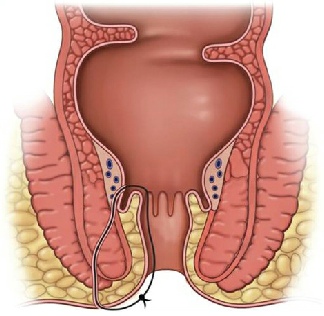
- Seton suture. A Seton suture or Seton drain is a piece of thread or silastic sloop which is left in the fistula tract. This may be considered if you are at high risk of developing incontinence when the fistula crosses the sphincter muscles. Sometimes several operations are necessary. Gradually tightening the Seton suture so that it slowly cuts through the fistula
- Rectal advancement flap. This option is usually when the fistula is considered complex, or is there is a high risk of incontinence. The advancement flap is a piece of tissue that is removed from the rectum or from the skin around the anus. During surgery, the fistula tract is removed and the flap is reattached where the opening of the fistula was. The operation is effective in about 70% of cases.
- Fibrin glue. This is currently the only non-
surgical treatment option. The glue is injected into the fistula to seal the tract, then the opening is stitched closed. It is a simple, safe and painless procedure, but long term results for this method are poor. Initial succes  s rates as high as 77% drop to 14% after 16 months.
s rates as high as 77% drop to 14% after 16 months. - Bioprosthetic plug. This is a cone shaped plug made from human tissue, which is used to block the internal opening of the fistula. Stitches keep it in place. However, this does not completely seal the fistula, so that it can continue to drain. New tissue usually grows around the plug to heal the fistula. Two trials show success rates of over 80% for this method, but long term success rates are uncertain.
- LIFT procedure (Ligation of the Intersphincteric Fistula Tract)
Most of the time, fistula surgery can be performed on an outpatient basis. Treatment of a deep or extensive fistula may require a short hospital stay.
How long does it take before patients feel better?
Discomfort after fistula surgery can be mild to moderate for the first week and can be controlled with pain pills. The amount of time lost from work or school is usually minimal.
Treatment of an abscess or fistula is followed by a period of time at home, when soaking the affected area in warm water may help. Stool softeners (e.g. lactulose) or a bulk fibre laxative (e.g. Fybogel) may also be recommended. It may be necessary to wear a gauze pad or mini-
What are the chances of a recurrence of an abscess or fistula?
If properly healed, the problem will usually not return. However, it is important to follow the directions of a colon and rectal surgeon to help prevent recurrence.
Are there any long-term effects of surgery for a fistula in ano?
There is a risk of complications after anal fistula surgery, including:
- Infection
- Bowel incontinence
- Recurrence of the anal fistula (i.e. the fistula comes back)
For example, after the most common type of surgery for a fistula (known as a fistulotomy), the risk of an anal fistula coming back is around 21%. The risks vary depending on the type of procedure. You can discuss this with your surgeon.
In a very few cases if someone has weak muscles around the back passage (anal sphincter) and a tendency to difficulty in controlling the bowels, or leakage, this may worsen after the operation. If you find that you are having difficulties talk to your doctor.
Can I be treated for an anal abscess or fistula at the Glasgow Colorectal Centre?
Yes. Glasgow Colorectal Centre surgeons Richard Molloy and Graham MacKay are experienced in the management of patients with perianal abscesses and fistulas.
An anal (perianal) abscess is an infected cavity filled with pus found near the anus or rectum. An anal fistula is a track or tunnel between the skin on the outside of the buttock/anal area and the anal canal on the inside. There are many different types of fistulae from relatively simple to a complex branching network of tracks. Some fistulae may involve the muscles responsible for bowel control. Each fistula is individual.